Mechanical Ventilation in the ICU: Facts and Figures
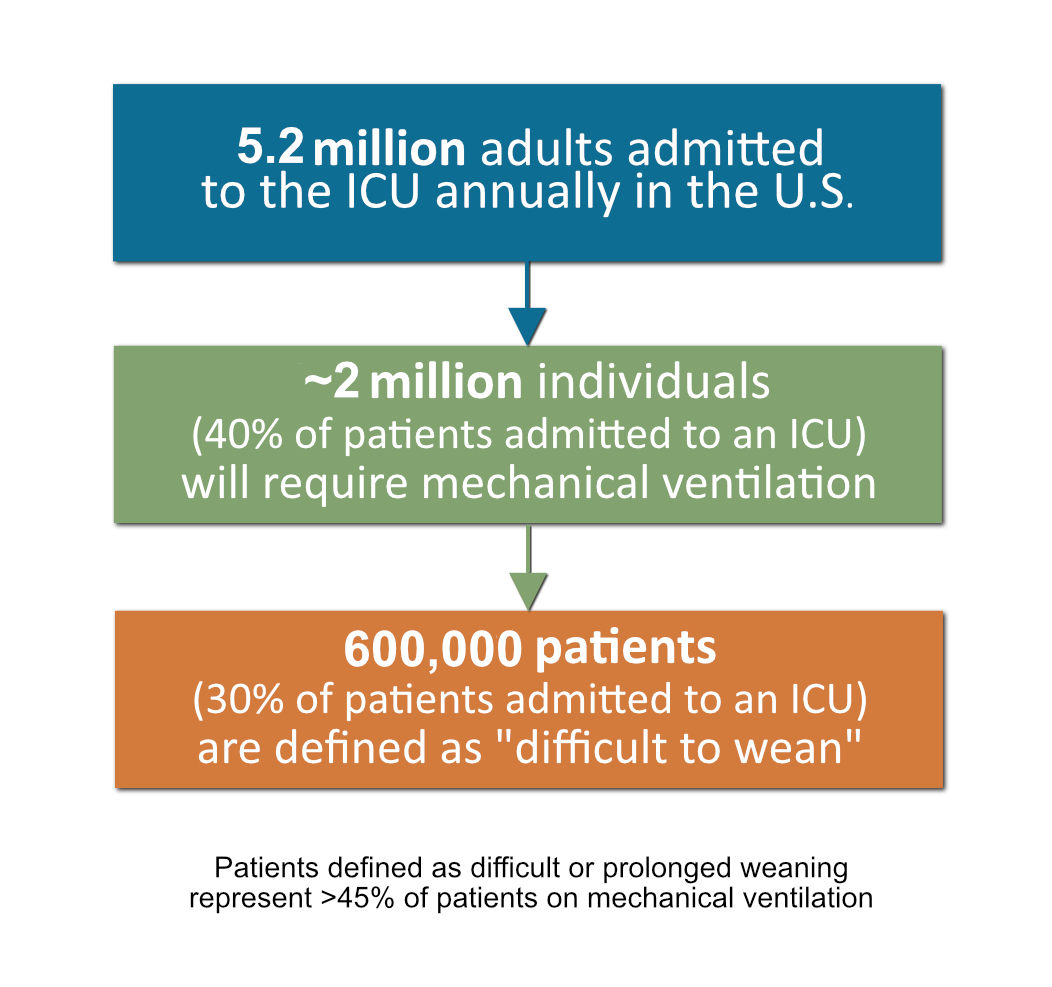
- Mechanical ventilation is one of the most common interventions implemented in the ICU.1
- 39.5% of ICU admissions require mechanical ventilation.2
- Over 2 million hospitalizations annually in the U.S. include the use of mechanical ventilation.3
- The mean length of stay for ventilated patients is 14.1 days.4
- The mean total hospital costs for patients who receive mechanical ventilation are $34,000 per stay.5
- Estimated annual mechanical ventilation-associated costs are >$27 billion, representing 12% of total hospitalization costs.4
- In hospital mortality for ventilated patients is 34.5%.4
- 30% of patients experience difficult or prolonged weaning.6-12
- Only 30.8% of patients on ventilators are discharged home from the hospital.4

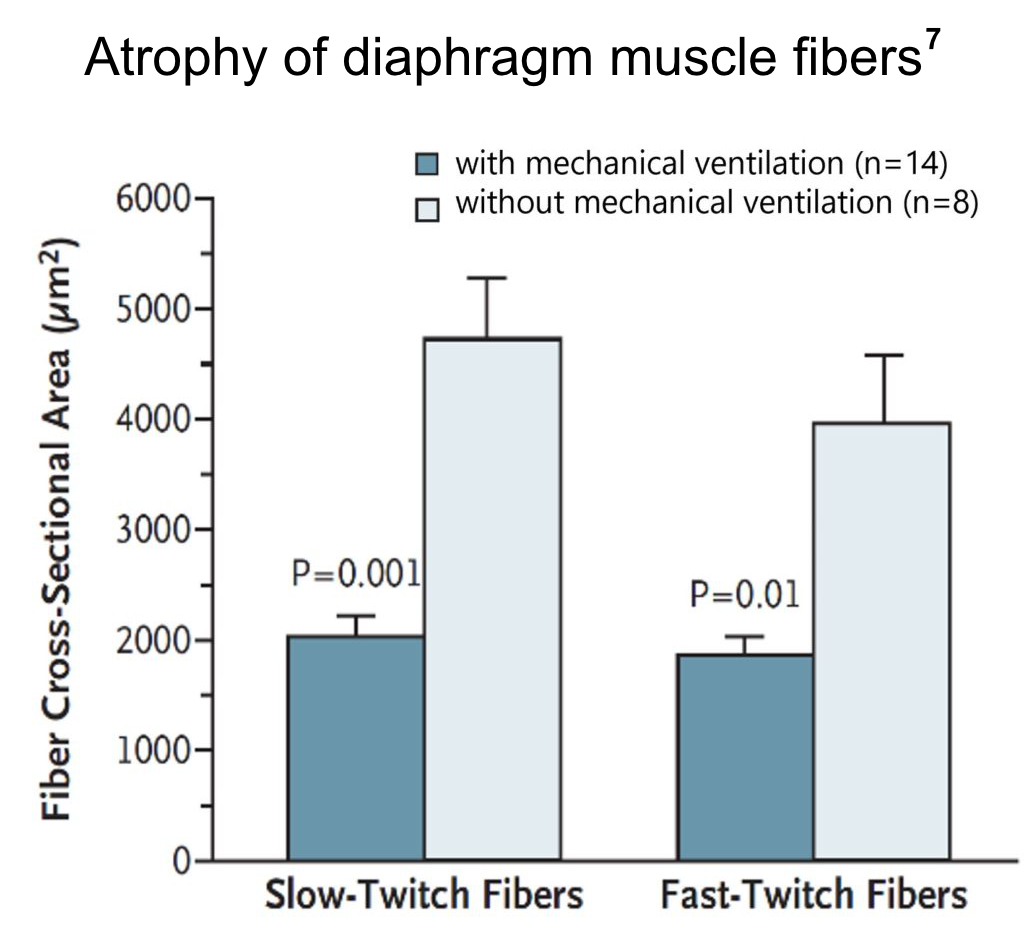
Mechanical ventilation rapidly produces diaphragm atrophy
Mechanical ventilation is a vital and effective therapy; however, it frequently leads to lung injury, diaphragmatic weakness, ventilation-induced diaphragmatic atrophy, and injury. Research has indicated that the combination of diaphragmatic inactivity and extended mechanical ventilation (lasting more than 18 hours) is linked to muscle fiber atrophy in the diaphragm. This condition is referred to as “Ventilator-Induced Diaphragmatic Dysfunction” or “VIDD.”
VIDD has been shown to contribute to problems in weaning patients from mechanical ventilation. This extended time on the ventilator increases health care costs and greatly increases patient morbidity and mortality.
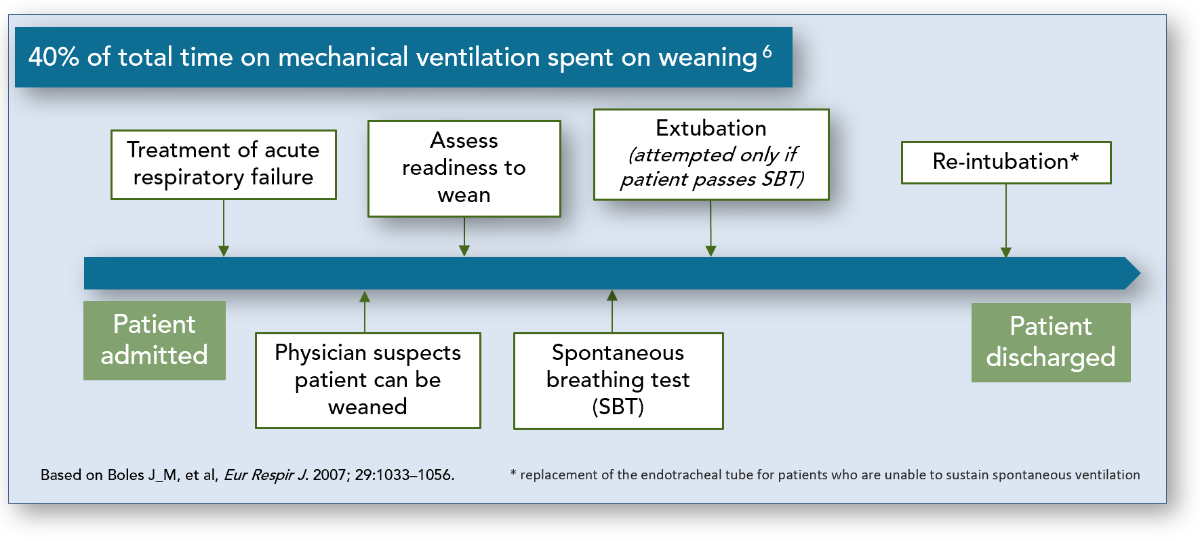
“Weaning” is defined by the gradual process of decreasing ventilator support. The first step in the weaning process is a spontaneous breathing trial (SBT) and is initiated when a physician suspects the patient can be weaned. A SBT is utilized to assess the patient’s ability to breathe while receiving minimal or no ventilator support. If a patient passes a SBT, extubation is attempted. Often times a patient requires reintubation and continued mechanical ventilation even if they have passed a SBT. It is estimated that 40% of the duration of mechanical ventilation is dedicated to the process of weaning.2
While delayed weaning can lead to complications such as ventilator induced lung injury, pneumonia, and VIDD, premature attempts at weaning can also lead to complications including loss of the airway, defective gas exchange, aspiration and respiratory muscle fatigue.
Classification of Patients by Weaning Status
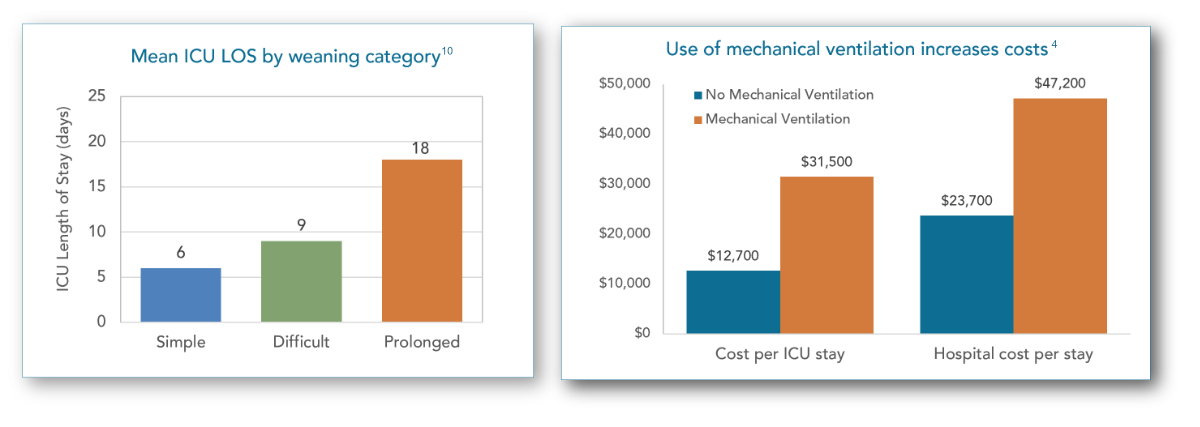
An International Consensus Conference created a classification system which assigned patients into one of three groups based on difficulty and length of the weaning process.10 This includes:
- Simple weaning – patients proceeds from initiation of weaning to successful extubation on the first attempt without difficulty.
- >Difficult weaning – patients who fail initial weaning and require up to three spontaneous breath tests (SBT) or as long as 7 days from the first SBT to achieve successful weaning.
- Prolonged weaning – patients who fail at least three weaning attempts or required >7 days of weaning after the first SBT.
The graphic to the left summarizes the total annual patient population in the U.S. who are admitted to an ICU and are placed on mechanical ventilation. This graphic also provides estimates for the number of patients who fall into each of the above weaning categories.
The Economics of VIDD
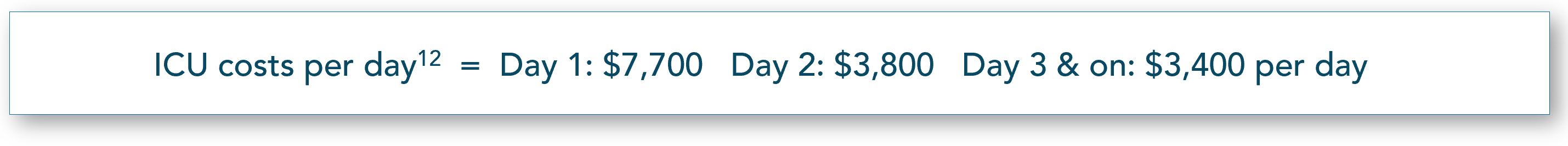
Prolonged weaning time increases a patient’s length of stay in the ICU and also contributes to increased hospitalization costs.6,10 Extended time in the ICU also increases the risk of developing hospital associated infections (HAIs) and other complications.
“Due to its intrusiveness and duration of use, invasive ventilation is associated with increased risk of complications such as pneumothorax, ventilator-associated pneumonia, decreased cardiac output, oxygen toxicity and acute lung injury or acute respiratory distress syndrome.” 9
References
- American Association for the Surgery of Trauma. http://www.aast.org/GeneralInformation/mechanicalventilation.aspx. Accessed October 2018.
- Esteban A, Ferguson ND, Meade MO, et al. Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med. 2008;177:170–177.
- Boles JM, Bion J, Connors A, et al. Weaning from mechanical ventilation. Statement of the Sixth International Consensus Conference on Intensive Care Medicine. Eur Respir J. >2007: 29:1033-56.
- Wunsch H, Wagner J, Herlim M, Chong DH, Kramer AA, Halpern SD. ICU occupancy and mechanical ventilator use in the United States. Crit Care Med. 2013; 41:2712-9.
- Wunsch H, Linde-Zwirble WT, Angus DC, et al. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010 Oct;38(10):1947-53.
- Donahoe MP. Current venues of care and related costs for the chronically critically ill. Respir Care. 2012; 57:867-86.Levine S, Nguyen T, Taylor N, et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med. 2008; 358(13):1327-35.
- Levine S, Nguyen T, Taylor N, et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med. 2008; 358(13):1327-35.
- unsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med. 2008; 36:2787-93.
- National Institutes of Health. National Heart,Lung and Blood Institute. https://www.nhlbi.nih.gov/health-topics/ventilatorventilator-support. Accessed October 2018.
- Peñuelas O, Frutos-Vivar F, et al. Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am J Respir Crit Care Med. 2011;184:430-7.
- Zilberberg MD, Shorr AF. Prolonged acute mechanical ventilation and hospital bed utilization in 2020 in the United States. BMC Health Serv Res. 2008; 8:242.
- Donahoe MP. Current venues of care and related costs for the chronically critically ill. Respir Care. 2012; 57:867-86